How do people catch bird flu?

As bird flu infections rise in dairy cattle and chickens, human cases are ticking up too, leaving many people to wonder whether they might be at risk from this recently arrived virus.
Bird flu infections are rare in people. Sixty-one human cases have been confirmed in the US this year, according to the US Centers for Disease Control and Prevention, and all but three have been in people who work on poultry or dairy farms.
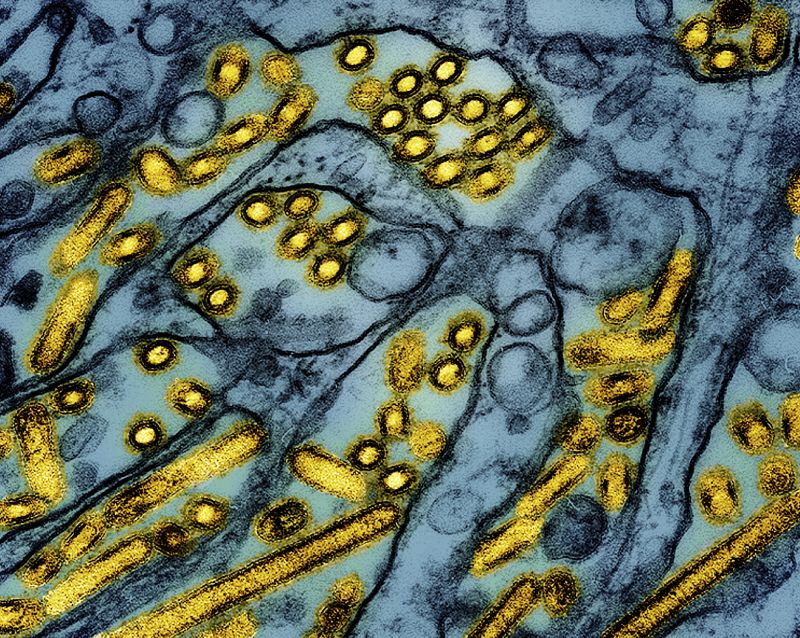
As the name suggests, avian influenza viruses prefer to infect birds. They break into cells by latching onto sugars that stick up from their surfaces called sialic acids. H5N1, the bird flu virus behind the ongoing outbreak in the US, has really only demonstrated an affinity for the types of sialic acid receptors that are most plentiful in the respiratory tracts of birds.
But flu viruses can also mutate quickly, and since 2022, H5N1 has been infecting a growing variety of mammals, including dairy cattle.
That has scientists on alert because the more it circulates in animals, the better it gets at finding new hosts.
A study published last week in the journal Science showed that just one key change to the virus’ genetic material would allow it to attach to the kinds of sialic acids that are most common in the nose and lungs of people. But it’s nearly impossible to predict when that could happen — or if it ever will.
Animal-to-human spillover events
When humans have become infected with bird flu, it’s almost always been through contact with infected animals. All but one of these so-called spillover infections have been mild.
The United States’ first severe case was announced this week in a person in Louisiana who remains hospitalized in critical condition. The CDC said Wednesday the person was exposed to sick and dead birds on their property, not from commercial poultry.
No one who has gotten H5N1 in the US is known to have given the infection to anyone else. For that reason, the CDC estimates that the current risk to the public is low, but there are certain occupations and situations that can increase a person’s risk of catching bird flu.
The two groups of people who are most at risk are farm workers who work with cows or poultry and people who keep backyard flocks, said Dr. Michael Osterholm, who directs the Center for Infectious Disease Research and Policy at the University of Minnesota.
Birds shed the virus through their saliva, mucus and feces, and it can become airborne when their litter and feathers are churned up in barns, particularly during culling operations.
“It can be in the air,” Osterholm said. “So it’s not even just contact touching the birds but just the dander and all the dust that occurs when you’re dealing with birds.”
The virus also homes in on the udders of milking cows, and studies have found high concentrations of bird flu virus in milk that is raw or unpasteurized.
The milking parlors of dairies are wet environments, and workers can be infected if they get a splash of raw milk in their eyes or if they get milk on their hands and then rub their eyes. Droplets of virus-laden milk can also become airborne if they spray from milking equipment.
One of the most prominent symptoms in infected farm workers has been red, irritated eyes, or conjunctivitis. That may be because human eyes share the same types of sialic acid receptors that are most common in birds.
Risks from raw milk
What about drinking raw milk?
Cats have been infected after drinking raw cow’s milk. There have also been reports of calves getting sick after drinking infected milk.
“We don’t have those same data for humans,” Osterholm said.
No human infections have been linked to raw milk consumption, although a toddler in California recently tested positive for influenza after drinking a large amount of raw milk. The CDC wasn’t able to confirm whether the infection was bird flu, however, so this child is listed as a suspected case.
But there’s plenty of data on other pathogens that can be found in raw milk, even without specific evidence for H5N1. In 2023 and 2024, outbreaks of E. coli and salmonella infections were traced back to raw milk. It can harbor other pathogens like listeria and Campylobacter, too.
Pasteurization kills all these harmful germs, including H5N1, a recent government study shows.
However, refrigeration does not. A recent study from Stanford University that involved lacing raw milk with flu virus and testing it on cells in a Petri dish found that the virus could still infect cells for up to five days after being refrigerated.
Staying safe
The best way to protect yourself from bird flu is to avoid sources of exposure, according to the CDC.
- Sign up here to get The Results Are In with Dr. Sanjay Gupta every Friday from the CNN Health team.
People can catch bird flu when enough virus gets into their eyes, nose or mouth or when they breathe it in. This usually takes close, prolonged exposure to infected animals.
For that reason, the CDC recommends that people stay away from sick or dead birds or other animals, and avoid touching surfaces contaminated with feces or saliva, such as litter or bedding.
If you do have to handle sick birds, cows or other animals, such as in a farm or rescue setting, the CDC recommends wearing appropriate personal protective equipment, or PPE. This includes:
- Goggles
- Disposable gloves
- An N95 face mask
- Coveralls
- Rubber boots
Because raw milk can carry so many dangerous germs, experts advise avoiding it and sticking to pasteurized dairy products.
But what about raw eggs? The US Food and Drug Administration says it’s unlikely that eggs from an infected flock would make it onto store shelves because birds rapidly become sick from bird flu, and there are safeguards in place, such as inspections, to prevent contaminated eggs from reaching the market.
It’s still a good idea to cook eggs and poultry to a safe temperature and prevent cross-contamination between raw and cooked foods in the kitchen.